Heart Electrical System Anatomy and Sequence of Electrical Conduction
Learn More About Simplified Science PublishingThe heart electrical system is controlled by the spread of electrical signals between specialized cells in the heart muscle. They follow a consistent pattern that can be measured using tools such as the electrocardiogram (ECG).
What is heart electrical conduction?
The heart electrical conduction anatomy is made up of a network of signaling pathways that control your heartbeat. Each time your heart pumps blood throughout your body, electrical signals travel through different areas of your heart that make your heart chambers expand or contract. This electromechanical pumping mechanism is carefully timed to allow for consistent blood flow and blood pressure.
Note: If you are not familiar with basic heart anatomy, I suggest you read the heart structure and function article first.
Sequence of electrical conduction through the heart
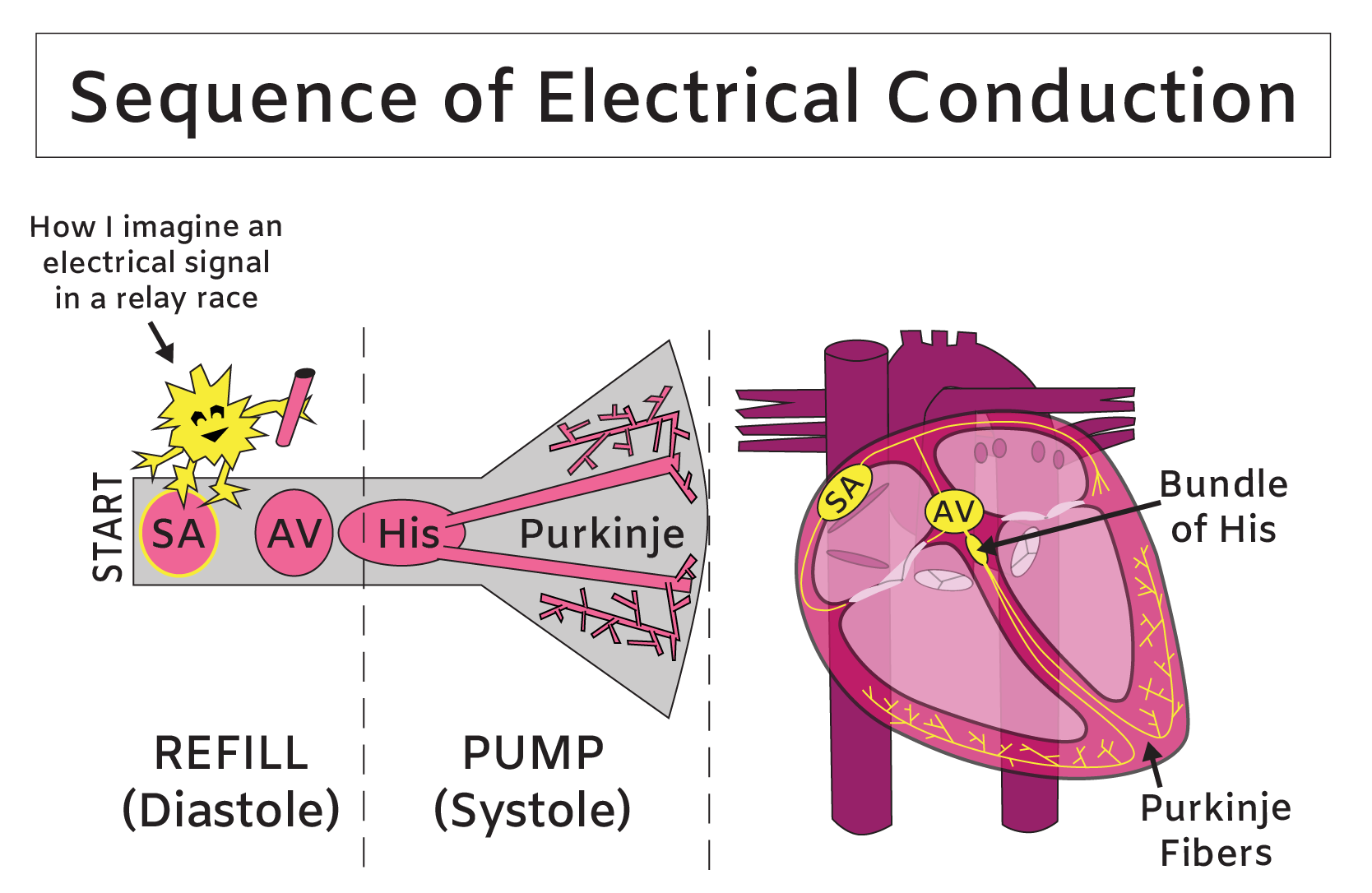
The heart sequence of electrical conduction starts in the upper-right wall of the right atrium where specialized cells form a cluster called the sinoatrial (SA) node. The SA node is known as the heart’s pacemaker and it creates the starting signal for each heartbeat. When the SA node triggers an electrical pulse, it sends electrical messengers racing toward left atrium and toward the second important cell cluster, called the atrioventricular (AV) node. The AV node is located in the lower-left side of the right atrium and the electrical activity between the SA and AV segment of the race causes the muscles of both the left and right atria to contract, which helps push blood from the atria into the ventricles.
After a brief rest to allow the ventricles to fill with blood, the electrical baton is handed from the AV node to a narrow group of Purkinje cells called the bundle of His. From here, the electrical racers split off in two directions: half head down the track toward the right ventricle and the other half race toward the left ventricle. The final hand-off occurs at the base of the ventricles, where the electrical impulse is sent through thin Purkinje fibers on both sides of the heart. The final sprint through the Purkinje fibers causes the muscular walls of the ventricles to contract, which pumps blood from the right ventricle into the lungs and from the left ventricle out into the body. At this point, the heartbeat is complete and the electrocardio relay race starts up again from the SA node.
You can think of the heart’s electrical conduction system as an electric relay race, where the electrical baton is passed between groups of cells that make different regions of the heart contract at different times.
Each heartbeat is created by muscle contractions that squeeze the chamber walls in a precise pattern. These muscle contractions provide the force that pumps blood throughout your body, similar to a foot pump that forces air into your favorite floating device. But instead of pumping air into toys for a pool party, your heart functions as a dual blood pump to support your life party. The “dual” part of the blood pump arises because the right and left sides of your heart function as separate pumps that send blood to two different destinations: the lungs and the body. The right chambers of your heart receive deoxygenated blood from your body’s veins and pump it into your lungs and the left chambers of your heart pump the recently oxygenated blood into the rest of your body.
Heart arrhythmias and treatments
A heart arrhythmia occurs when a heart is beating too fast, too slow, or when there is a problem with a heart’s pattern of refill and pump. A person can be born with an irregular heartbeat, but arrhythmias can also occur when damaged or aging heart tissue prevents electrical signals from making smooth and properly paced laps around the electrocardio racetrack. The fact that the heart has a self-contained electrical system has allowed for the development of useful medical treatments, such as the defibrillator and the artificial pacemaker. Both of these devises can help a patient whose heartbeat has an irregular rate or rhythm.
Most arrhythmias are not life-threatening. However, if an irregular heartbeat impairs the pumping of blood into the lungs and the rest of the body, it can have immediate and deadly consequences. The cells in the human body require a constant supply of oxygen and if the heart’s chambers are not contracting at the right times or if they are not contracting strongly enough, it can result in a dangerous decrease blood flow and oxygen delivery. Without proper oxygen delivery, a person can pass-out and die within minutes. Therefore, it is essential that you pay attention to your blood pump and seek immediate medical care if you sense an abnormality in your heartbeat’s rate or rhythm.
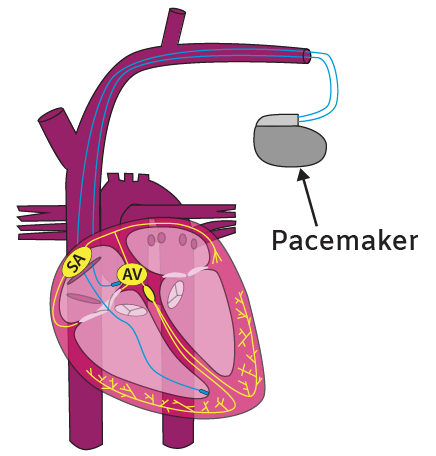
How does a pacemaker work?
If a person has a heart arrhythmia that disrupts blood flow, a doctor may suggest a surgery to implant a defibrillator or a pacemaker to monitor and control the heart’s electrical impulses. These devices are implanted under the skin in the upper chest and have wires that are guided through a vein and into the heart. The tips of the wires are both sensing and stimulating electrodes. They detect irregular heart contractions and then send electrical pulses to override and correct the abnormality with each heartbeat.
The first defibrillators and pacemakers that were used for clinical research in the 1950s were large external devices that needed to be wheeled around on carts and plugged into an electrical outlet. Today’s implantable heart devices are automated, battery powered and roughly the size of a packet of gum. Thank you, research and technology.
Electrocardiograms (ECG or EKG)
In addition to controlling a person’s heartbeat with external electricity, medical professionals who are concerned with a heart’s function can also stick electrodes to a person’s chest and limbs to measure the details of a person’s heartbeat. Electrodes that are placed in specific locations on the skin can detect the heart’s electrical pattern and generate a graph called an electrocardiogram (EKG or ECG). You may be familiar with this graph if you watch medical television dramas because an ECG often indicates the death of a fictional patient when the graph “flatlines” to show that the patient’s heart has lost all electrical activity. But the ECG is more than just a tool to determine whether the heart is electrically dead and a close look at the squiggles can reveal important information about a heart’s function.
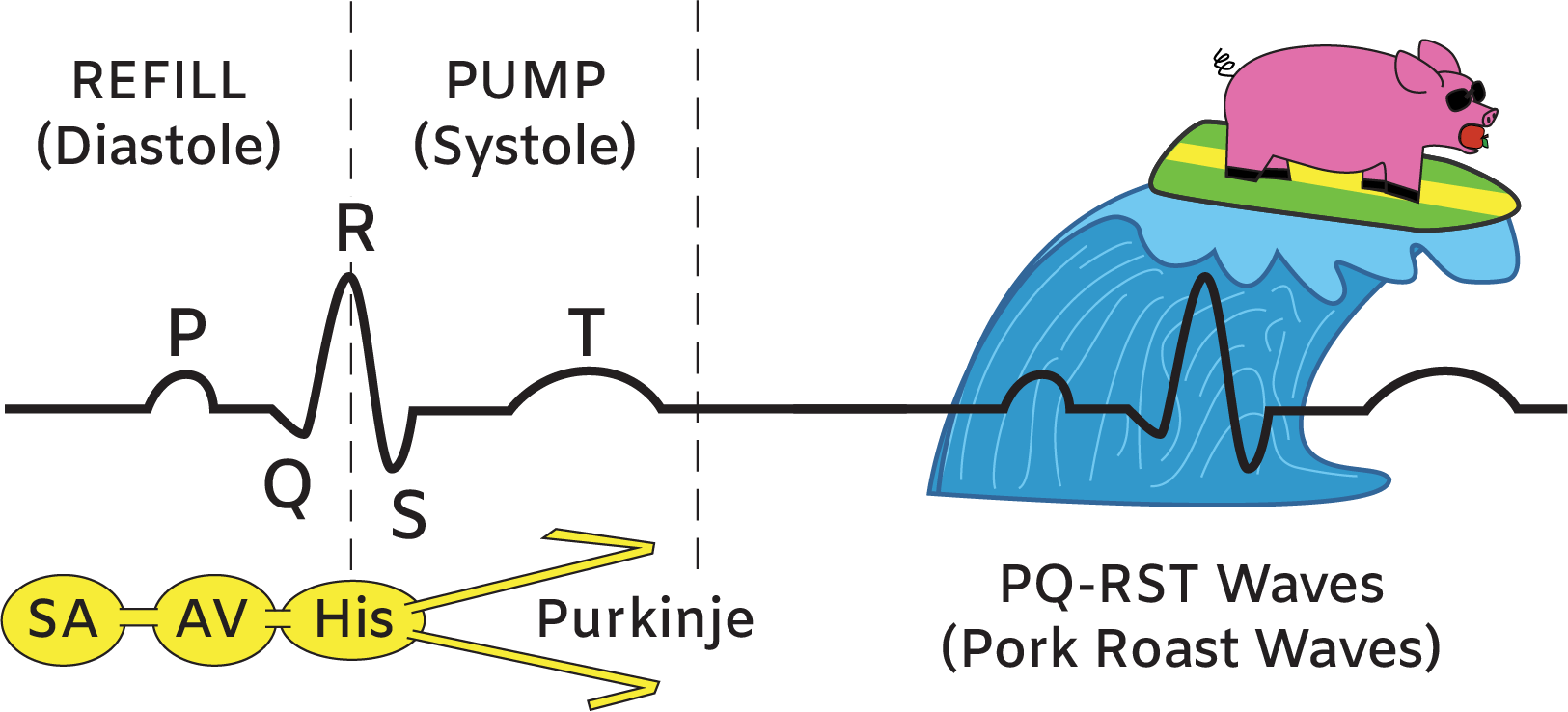
An ECG depicts the sequence of electrical conduction. There are three main ECG peaks that are named the P wave, the QRS wave, and the T wave. To remember these details, you can think of the PQRST peaks as the Pork Roast Waves, where the Pork (PQ) represents the heart’s refill and the Roast (RST) loosely represents the pump. To be more precise, the 'P' wave is caused by the electrical activity between the SA and AV nodes and it results in an atria contraction that pushes blood into the ventricles. The 'QRS' complex shows the electrical activity from the AV node all the way to the Purkinje fibers in the ventricles, where the segment between the 'R' and the 'S' represents the muscle contraction of both ventricles. Finally, the 'T' wave shows that the electrical activity in the ventricles as they return to baseline. By analyzing the shape, height and timing of the PQRST waves, a doctor can use the ECG to diagnose many specific problems in a patient’s heart.
Human electrical conduction study guide
Heart Sequence of Electrical Conduction: Electrical signals move from the sinoatrial (SA) node to atrioventricular (AV) node in the atria, then move to a narrow group of Purkinje cells called the bundle of His and finally move to the Purkinje fibers in the left and right ventricles.
Heart Arrhythmias: Heartbeat with an irregular rate or rhythm.
Pacemaker: Device that detects irregular heart contractions and then send electrical pulses to override and correct the abnormality with each heartbeat.
Electrocardiogram (ECG or EKG): Tool that detects the heart’s electrical sequence of electrical conduction.
The heart is a powerful organ that tirelessly moves five to six liters of blood on a full tour of your body nearly every minute. Because of this essential function, it is one of the most important organs for human health. Consider donating to help fund lifesaving research and advocate for better heart health for at-risk populations.
Related Content:
- How Does the Heart Work? Review Heart Structure and Function
- What is a Heart Attack? Heart Attack Causes and Prevention Tips
- What is Blood Made Of? Review Blood Components and Functions
- What is Aerobic Respiration and Why is it Important?
- How Does the Diaphragm Work? Diaphragm Structure and Function
References:
- Harrison's Principles of Internal Medicine, 18th Edition. Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson J, Loscalzo J. eds.
- Anatomy, Physiology, and Disease: An Interactive Journey for Health Professions , 2nd Edition. Bruce J. Colbert, University of Pittsburgh, Johnstown.
- https://www.thehealthy.com/bodies/human-body-every-minute/
Create professional science figures with illustration services or use the online courses and templates to quickly learn how to make your own designs.
Interested in free design templates and training?
Explore scientific illustration templates and courses by creating a Simplified Science Publishing Log In. Whether you are new to data visualization design or have some experience, these resources will improve your ability to use both basic and advanced design tools.
Interested in reading more articles on scientific design? Learn more below:
Content is protected by Copyright license. Website visitors are welcome to share images and articles, however they must include the Simplified Science Publishing URL source link when shared. Thank you!